How US and UK Doctors and Nurses Can Move from Clinical Practice into Digital Health (Without Starting Over)
Written by Rod on February 9, 2026
Many US and UK doctors and nurses feel trapped in a paradox: they still care deeply about patients, but clinical practice has become unsustainable. Chronic understaffing, endless administrative burden, and repetitive routines have eroded the joy you once felt at the bedside. At the same time, you’ve noticed you actually enjoy fixing broken workflows, championing your electronic health record, or testing new AI documentation tools during ward rounds. The transition from clinical practice to digital health no longer needs to feel risky or unclear—this guide lays out a proven roadmap showing exactly how to leverage your clinical expertise for roles offering better work-life balance, intellectual stimulation, and competitive pay, all without starting your career over.
Yet the leap to digital health still feels risky and unclear.
How do you transition from clinical practice to digital health without throwing away ten-plus years of training? How do you move into a role that offers better work-life balance, intellectual stimulation, and competitive pay — without starting again at the bottom?
This guide lays out a clear, realistic roadmap so you can see exactly where you are today, what realistic next steps look like, and how to reduce financial, professional, and identity risks as you move from purely clinical work into meaningful digital health roles.
Why doctors and nurses are moving into digital health
Burnout remains the number-one driver. Recent 2025–2026 surveys (Medscape, GMC, RCN, NHS Staff Survey) continue to show 45–60% of clinicians experiencing moderate to severe burnout. At the same time, the digital health sector has become one of the few areas in healthcare that is growing rapidly and actively recruiting people with deep clinical insight.
Key reasons clinicians are making the move in 2026:
– **Desire for sustainable careers** — fewer nights, fewer emotional extremes, more control over schedule
– **Opportunity to influence at scale** — instead of improving care for one patient at a time, you can help redesign systems that affect thousands
– **Better long-term earning potential** — many digital health roles now match or exceed senior clinical salaries, especially in informatics, clinical safety, and industry
– **Intellectual renewal** — working with AI tools, virtual care pathways, ambient documentation, and workflow optimisation feels more future-facing than endless rota gaps
– **Flexibility & remote options** — particularly attractive for nurses and doctors with young families or those wanting to reduce physical and emotional load
The digital health market continues to expand — projected to exceed $1 trillion globally by 2030 — and organisations increasingly realise they cannot build safe, usable products without clinicians in key roles.
What “digital health” actually means for clinicians
Digital health is not “tech for tech’s sake”. For doctors and nurses, it means using technology to make care safer, faster, more equitable, and less exhausting.
Common areas in 2026 include:
– Optimising and configuring EHR / EPR systems (Epic, Cerner, SystmOne, EMIS, etc.)
– Designing and implementing clinical decision support, AI ambient scribes, and generative AI tools
– Building or improving virtual wards, remote monitoring, and telehealth pathways
– Leading digital transformation projects inside hospitals and integrated care systems
– Working in health-tech companies as clinical advisors, product specialists, or medical directors
– Contributing to clinical safety, governance, and risk assessment of digital tools
You do **not** need to become a software engineer. The most valuable clinicians in digital health are those who can translate messy frontline reality into clear requirements, spot safety risks early, and keep patient care at the centre of technology decisions.
A simple roadmap: from curious clinician to digital health role
Here is a practical four-phase progression that thousands of clinicians have followed successfully.
Phase 1 – Curiosity & Awareness (0–3 months)
Goal: Understand the landscape without changing your current job.
Actions:
– Read industry updates (Digital Health.net, HSJ Digital, Healthcare IT News, MedTech Dive)
– Join relevant LinkedIn groups and X communities (#digitalhealth, #healthinformatics, #clinicalinformatics)
– Complete 1–2 short free courses (NHS Digital Academy modules, Coursera “AI in Healthcare”, FutureLearn health informatics)
– Speak to 2–3 people already in digital roles (many are happy to do 15-minute informal chats)
Phase 2 – Low-risk Experience Building (3–9 months)
Goal: Gain credible experience while still clinical.
Actions:
– Volunteer as a digital / super-user / EPR champion in your organisation
– Join internal quality improvement or AI pilot projects
– Document your contributions (before/after metrics, screenshots of workflows you improved)
– Start building a simple portfolio (LinkedIn posts, short case studies)
Phase 3 – Positioning & Networking (6–15 months)
Goal: Become visible to external employers.
Actions:
– Update LinkedIn headline and summary with digital keywords
– Attend 1–2 conferences (HIMSS, HLTH, Digital Health Rewired, CCIO Summer School)
– Apply for part-time / secondment roles (e.g., 1 day/week clinical informatics)
– Complete a recognised certification if appropriate (CHIME, NHS Digital badges, Epic Proficiency, FHIR basics)
Phase 4 – Transition (9–24 months)
Goal: Secure a sustainable digital health role.
Actions:
– Target full-time roles: clinical informaticist, digital fellow, CNIO/CMIO pathway, industry clinical lead
– Use your portfolio and internal experience to demonstrate value
– Negotiate flexible or remote arrangements where possible
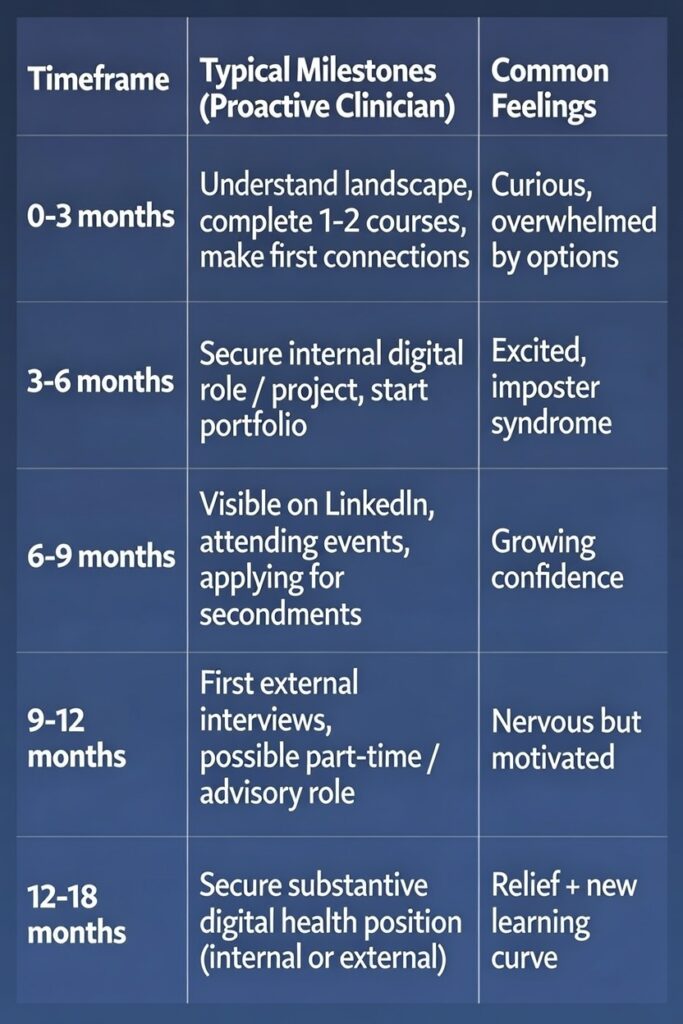
How long does it take to move into digital health?
Most clinicians who are proactive achieve a meaningful shift within 9–18 months. Those who secure internal secondments or part-time industry advisory work can move faster.
How to reduce risk: income, licence, and career identity
Income protection
– Keep clinical sessions (bank / locum / private work) during transition
– Target roles with salaries comparable to or higher than your current pay (many informatics and industry roles start at £80–130k / $120–200k+)
– Build a small financial buffer (3–6 months expenses) before going full-time
Licence & registration
– UK: Maintain GMC / NMC registration via CPD and revalidation (digital work usually counts)
– US: Keep state license and board certification active (many roles offer CME allowance)
– Most digital health employers value an active licence even if you are no longer practising full-time
Career identity
The shift from “bedside clinician” to “clinical digital leader” can feel strange at first. Reframe it as:
“I’m still a doctor/nurse — I’m just using my expertise to improve care for many more patients.”
Timelines: what to expect over 6–12 months (2026 reality)
Factors that accelerate progress in 2026:
– Working in a digitally mature organisation (e.g., Epic/Cerner trust, large US health system)
– Early involvement in AI or virtual ward projects
– Strong LinkedIn presence and network
Next steps if you want help designing your transition
You don’t have to figure this out alone.
Here are immediate, low-effort actions you can take this week:
– Download my free “Clinician to Digital Health Readiness Checklist” at rodgamble.com
– Join the weekly newsletter for current role alerts, project opportunities, and short case studies
– Book a 30-minute discovery call if you want personalised feedback on your next 90 days
The demand for clinicians who understand both patients and digital systems is higher than ever. You already have the hardest part — real-world clinical experience. The rest is learnable, step by step.
You’ve spent years mastering medicine and nursing.
Now you can use that expertise to help fix healthcare at a systemic level — without having to start your career over.